Acute coronary syndrome
Definition

A set of symptoms and signs compatible with ischaemic heart disease.
Important terms
- Infarction - death of tissue due to a lack of oxygen.
- Myocardial - pertaining (big word) to heart muscle. Thus a myocardial infarction is death of heart muscle due to lack of oxygen.
- Ischaemia - lack of blood supply causing dysfunction of tissue
- Angina (full term is angina pectoris) - chest pain caused by ischaemia
Why don't we just call it a heart attack?
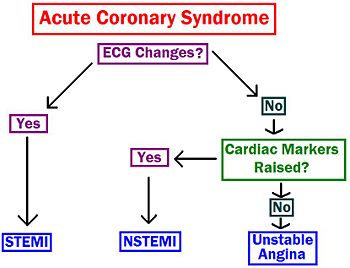
The problem is that the features that are typical of a myocardial infarction (MI) - colloquially known as a heart attack - aren't necessarily an MI. Essentially it's classified as the following:
- Unstable angina - angina which lasts longer that 10 minutes; severe and new onset; or distinctly more severe/prolonged than previous angina. Diagnosed by symptoms with NO rise in cardiac markers.
- Myocardial infarction is diagnosed by a rise in cardiac markers. It is further split into two types based on ECG changes.
- NSTEMI (non-ST elevation MI) - myocardial infarction where the ST segment of the ECG is not elevated
- STEMI (ST elevation MI) - MI where the ST segment is elevated. Please tell me you figured that out for yourself. If you didn't, give up medicine. Now.
Everyone of these conditions can potentially present with similar clinical features. They are only differentiated through further testing.
Epidemiology
Coronary heart disease is responsible for 15% of deaths in the UK. It's a big killer which is why it's important to know about. It's basically as important as cancer.
Pathophysiology
Over time, everybody builds up atherosclerosis in their veins. The atherosclerotic plaques rupture forming clots. These occlude the coronary arteries, stopping blood flow causing ischaemia and, if blocked for long enough, infarction. In angina only ischaemia occurs. In NSTEMIs, the vessel is not completely blocked but some heart muscle still dies.
Risk Factors
Take a look at ischaemic heart disease.
Clinical Features
- Chest pain - probably the defining one. Typically central, left-sided, crushing.
- radiating to left arm and neck
- Shortness of breath
- Nausea/vomiting
- Sweating
- Tachycardic, cold
- Sense of impending doom - did they feel like they were going to die?
30% of MIs are "silent" i.e. they are asymptomatic. These are more common in diabetes and elderly patients.
Investigations
There are two things you need to do with acute coronary syndrome: ECG and cardiac markers.
ECG changes
This is used to differentiate between a NSTEMI and a STEMI. Where there is ST elevation, with ACS symptoms, a STEMI can be diagnosed.
Acutely:
- The first changes seen are ST elevation and tall T waves. These occur in the first few hours.
- Within 24 hours the T waves invert and the ST elevation resolves.
- Q wave changes can occure within 24 hours or acutely. They are either wide (<0.04s) or to deep (<25% of the corresponding R wave).
Long term:
- Generally Q and T wave abnormalities are persistent. It's rare for ST elevation to remain.
In NSTEMIs, you can get ST depression and T wave inversion. (ST depression may also occur in a site opposite to that of the infarct.)
Cardiac markers
These decide between MI and unstable angina. There are two types:
- Troponin T (aka trop T) - is released by myocardium after infarction. Should be done 12 hours after the onset of symptoms. If done any sooner than 2 hours, it probably will not have risen significantly. Their presence is diagnostic of an MI.
- Creatinine Kinase (CK and CKMB) - CK is found in all muscle tissue so is less specific. CKMB is more specific to myocardium. Unlike Troponin, they can be done immediately. Often used as a screening tool, whilst waiting to do a Trop T.
Other investigations
These are to rule out rare causes of chest pain and ACS-like symptoms. Bloods:
- FBC - polycythaemia, anaemia
- U+Es - kidney function, electrolyte abnormalites (particularly hypokalaemia)
- LFTs - clotting abnormalities (because you're giving them thrombolysis)
- ESR/CRP - shows inflammation
- Lipid profile
- Clotting screen - clotting abnormalities (because you're giving them thrombolysis)
- Blood glucose
Imaging:
- CXR - heart failure and aortic dissection
- Echocardiography
- Angiography
- Myocardial perfusion scintigraphy
Management
Pre-hospital management.
- ABC: CPR and defibrillation if necessary
- In established ischaemic heart disease, call an ambulance where GTN spray fails. This is likely an MI rather than unstable angina
- Oxygen (high concentration)
- Aspirin 300mg
- Pain relief: 2.5-5mg diamorphine/5-10mg morphine IV
- Anti-emetic IV, with pain relief
- Insert venflon for bloods (see investigations)
- GTN (2 sprays, or 1 tablet)
In l'hopital (that's French, you know), there's a whole bunch of drugs you need to give them. Antiplatelet therapy in the form of clopidogrel for at least 4 weeks after a STEMI. Beta blockers and ACE inhibitors are both shown to also be beneficial post-MI. Heparin should be given to all patients subcutaneously; in some case it is given IV, usually with alteplase thrombolysis (not streptokinase) and before primary angioplasty.
Revascularisation

There are two types: PCI and CABG (pronounced cabbage - seriously).
- Percutaneous coronary intervention (aka PTCA: percutaneous transluminal coronary angioplasty) - what this involves is dilating the coronary arteries via insertion of a balloon catheter. A metallic stent is then placed inside the artery, holding it open.
- Coronary artery bypass graft - essentially a blood vessel from another part of the body is used to bypass the blockage in the coronary artery. Usually, the saphenous vein or the internal thoracic (aka internal mammary) is used.
Thrombolysis
Nowawdays, thrombolysis is less commonly done, PCI being the usual treatment. However, here's some details in case.
Thrombolysis is the use of drugs to break down clots (aka clot-busting). However, it's use limited as there is a specific timeframe for its administration. The main drugs are streptokinase, alteplase (given IV), reteplase and tenecteplase (given as rapid bolus injections). Streptokinase is the most common. The indications are:
- ST elevation (<1mm in <2 limb leads/<2mm in <2 chest leads)
- New onset left bundle branch block
- Within 12 hours; however, should be started ASAP and preferably within 1 hour
- Within 12-24 hours if continuing chest pain/continuing ST elevation/both
There is a large list of contraindications for thrombolysis: normal/no ECG; unconsciousness with no cause found; aortic dissection; intracranial pathology; pulmonary disease with cavitation; BP > 180/110; coagulation or bleeding problems; recent surgery; active GI problems (particularly bleeding); laser surgery on eyes; infective endocarditis; percarditis; pregnancy or 18 weeks postnatal; prolonged/traumatic CPR; previous allergy; and persistent antibodies to streptokinase.